Cystic Fibrosis: Helping Your Child Cough Up Mucus
Make an Appointment
Our team is here to help you make an appointment with the specialists that you need.
Top of the pageActionset
Cystic Fibrosis: Helping Your Child Cough Up Mucus
Overview
Draining mucus from the lungs and coughing it up can help to clear the lungs. Doing this every day can help your child maintain lung function and avoid problems from mucus.
Here are three ways to help clear your child's lungs. You may hear these called airway clearance techniques, or ACT.
- Postural drainage uses certain body positions to help clear different parts of the lungs.
- Chest and back percussion uses clapping (percussing) with a cupped hand, deep breathing, and then vibration to loosen and move mucus.
- Huffing and coughing . A huff is a forced breath. Huffing helps move mucus up in the lungs. Coughing moves it out.
It's important to keep using these techniques every day, even if you don't notice your child's lungs working better right away. Postural drainage, chest percussion and vibration, and huffing and coughing can work well when used regularly.
As your child gets older, they'll be able to do these techniques on their own. They may use a percussive vest or a positive expiratory pressure (PEP) device.
Your child's care team will make a personal treatment plan that includes airway clearance techniques. These therapies are one part of a larger treatment plan to help keep your child's lungs clear.
How can you help your child cough up mucus?
There are several ways you can help your child cough up mucus to clear their lungs. Talk to your child's doctor or respiratory therapist. They can show you and your child how to do each technique the right way.
Here's how you can help your child cough up mucus. To help prevent reflux from the stomach, make sure that your child's stomach is empty when you do this. Before a meal or at least an hour afterward is best.
- Set up items such as pillows and towels before you get started. You may need tissues, pillows, a thin cloth, or towels. Try different things to find the most comfortable place for you and your child to do the treatment. If you have a baby or small child, try sitting in a chair with them in your lap. An older child may do the treatment in bed.
- Position your child. Your child's doctor or therapist will recommend positions. Each position will help to clear a different part of your child's lungs. This technique is called postural drainage.
- Clap (percuss) your child's chest or back with your cupped hand. This loosens mucus and helps it move. Be sure the area is covered with thin clothing or a cloth. Form a "cup" with your hand. Clap on your child's chest or back at a quick and steady pace. When you clap, you should hear a hollow "popping" sound. If you hear a slapping sound, cup your hand more. Chest and back percussion are often used with postural drainage to help move the mucus.
- Use the right amount of force and a steady beat when clapping. How much force to use while clapping, and how long you clap, depends on your child. Here are some things to consider:
- Younger and smaller children need less force and time than older and larger children.
- Use enough force to help clear your child's lungs, but use less if you notice signs of pain and discomfort.
- Try using more force if your child is congested but mucus isn't coming up.
- Apply vibrations. This will help loosen and move mucus. At the end of each position, have your child take a big breath and blow it out slowly. As they blow out, place a flat hand over your child's chest or back area. Apply a little bit of pressure and quickly vibrate your arm and shoulder muscles.
- Have your child huff and cough. A huff is a forced breath that moves mucus higher in the lungs. This makes it easier to cough it up. Have your child take a deep breath in, hold it for 2 to 3 seconds, and then breathe it out through an open mouth with force (huff). It's much like breathing out to fog up a mirror. If any mucus comes up, have your child spit it out into a tissue.
Treatment usually takes 15 to 40 minutes per session. In general, a baby or small child who has no symptoms of congestion will need less treatment time than an older child who sounds congested and is coughing a lot.
At first, this may seem hard to do. But with help and practice, the treatment becomes easier, especially when you see that your child is breathing easier.
Positions to help your child cough up mucus
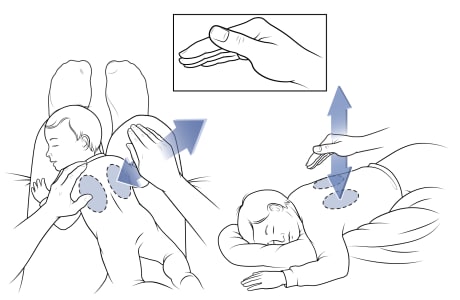
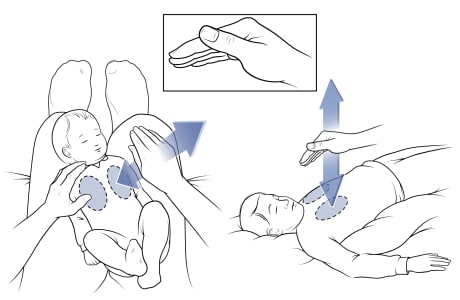
Hand position for percussion
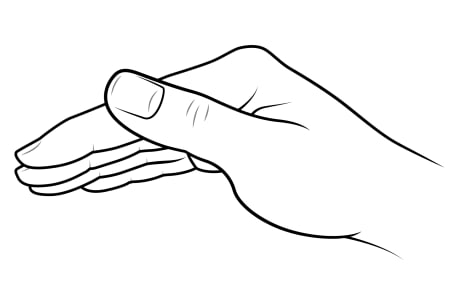
Form a "cup" with your hand. Start with a flat hand. Bend your hand slightly at your knuckles, and keep your index finger and thumb together. Use this hand position for percussion to help clear mucus.
Position for draining upper lobes (back)
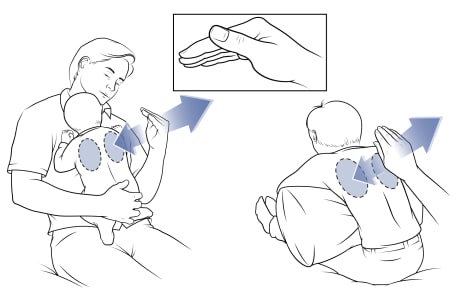
For infants: Lean back slightly (about 30 degrees) while resting your child's belly against your chest. Hold your child around the bottom to keep them steady. With the other arm, gently clap (percuss) between the spine and shoulder blade of the upper back. Clap for 1 to 3 minutes, depending on how much your child needs. Repeat on the other side of the spine.
For toddlers and older: Have your child lean forward slightly (about 30 degrees) on a pillow. Gently clap between the spine and shoulder blade of the upper back. Clap for 3 to 5 minutes. Repeat on the other side of the spine.
Position for draining upper lobes (front)
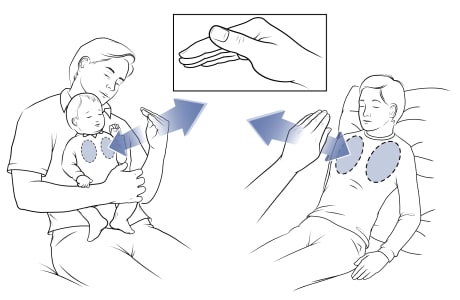
For infants: Lean back slightly (about 30 degrees) while resting your child's back on your chest. Hold your child around the waist with one arm to keep them steady. With the other arm, gently clap between the collarbone and nipple. Clap for 1 to 3 minutes. Repeat on the other side of the chest.
For toddlers and older: Have your child lean back slightly (about 30 degrees) on a pillow. Gently clap between the collarbone and nipple. Clap for 3 to 5 minutes. Repeat on the other side of the chest.
Position for draining lower lobes (sides)
For infants: Lay your child on their side, on your lap. Keep your child's head and upper body flat. To avoid reflux, do not place your child in a head-down position. Hold your child steady with one hand. With the other hand, gently clap below the armpit. Clap for 1 to 3 minutes. Repeat on the other side.
For toddlers and older: Have your child lie on their side. Gently clap below the armpit. Clap for 3 to 5 minutes. Repeat on the other side.
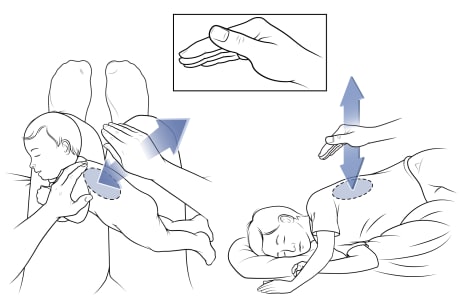
Position for draining lower lobes (back)
For infants: Lay your child on their stomach, on your lap. Keep your child's head and upper body flat. To avoid reflux, do not place your child in a head-down position. Hold your child steady with one hand. With the other hand, gently clap over the lower ribs. Clap for 1 to 3 minutes. Repeat on the other side of the back.
For toddlers and older: Have your child lie on their stomach. Gently clap over the lower ribs. Clap for 3 to 5 minutes. Repeat on the other side of the back.
Position for draining lower lobes (front)
For infants: Lay your child on their back, on your lap. Keep your child's head and upper body flat. Hold your child steady with one hand. With the other hand, gently clap on the front of the chest and just below the nipple. Clap for 1 to 3 minutes. Repeat on the other side of the chest.
For toddlers and older: Have your child lay on their back. Gently clap on the front of the chest and just below the nipple. Clap for 3 to 5 minutes. Repeat on the other side of the chest. If your child has developing breasts, put the heel of your hand under the armpit and clap with the fingers beneath the breast.
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.
To learn more about Ignite Healthwise, LLC, visit webmdignite.com.
© 2024-2025 Ignite Healthwise, LLC.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.



