Uterine Fibroids
Make an Appointment
Our team is here to help you make an appointment with the specialists that you need.
Uterine Fibroids
Condition Basics
What are uterine fibroids?
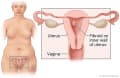
Uterine fibroids are growths on or in the uterus. Fibroids can grow on the outer wall, on the inner wall, or inside the wall of the uterus.
Your doctor may call them fibroid tumors, leiomyomas, or myomas. But fibroids aren't cancer. And they usually don't cause problems. You don't need to do anything about them unless they are causing problems.
What causes them?
Doctors aren't sure what causes fibroids. But the hormones estrogen and progesterone seem to make them grow. Your body makes the highest levels of these hormones during the years you have periods.
What are the symptoms?
Pain and heavy menstrual bleeding are the most common symptoms of uterine fibroids. But often fibroids don't cause any symptoms. Or symptoms may be mild, like periods that are a little heavier than normal. In some cases, having trouble getting pregnant is the first sign of fibroids.
How are they diagnosed?
To find out if you have fibroids, your doctor will ask about your symptoms. Your doctor will do a pelvic exam to check the size of your uterus. Your doctor may do an ultrasound or other tests to see inside your uterus. You may have blood tests to look for other problems.
How are uterine fibroids treated?
If you have fibroid symptoms that don't bother you or if you're near menopause, you may not need to do anything. If you have pain and heavy bleeding, try a nonprescription medicine like ibuprofen, or ask about other medicines. Procedures can also be done to help shrink or remove fibroids.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
What Increases Your Risk
Your risk for uterine fibroids increases as you age, especially from your 30s and 40s through menopause. But after menopause, fibroids usually shrink. Uterine fibroids are also more common in people who have a family history of fibroids, are Black, have high blood pressure, or are obese.
Symptoms
Uterine fibroid symptoms can develop slowly over several years or quickly over several months. Fibroids often cause mild symptoms or none at all. But sometimes the symptoms become a problem. The types of symptoms you have can depend on where the fibroid is found in the uterus.
Uterine fibroid symptoms and problems include:
- Abnormal menstrual bleeding.
This includes:
- Heavier, prolonged periods that can cause anemia.
- Painful periods.
- Spotting before or after periods.
- Bleeding between periods.
- Pelvic pain and pressure.
This includes:
- Pain in the belly, pelvis, or low back.
- Pain during sexual intercourse.
- Bloating and feelings of pressure in the belly.
- Urinary problems.
These include:
- Frequent urination.
- Kidney blockage following ureter blockage (rare).
- Other symptoms.
These may include:
- Difficult or painful bowel movements.
- Difficulty getting pregnant.
- Problems with pregnancy, such as placental abruption and preterm labor.
What Happens
Uterine fibroids can grow on the inside wall of the uterus, within the muscle wall of the uterus, or on the outer wall of the uterus. They can alter the shape of the uterus as they grow. Over time, the size, shape, location, and symptoms of fibroids can change.
Uterine fibroids are more common as you age, especially from your 30s and 40s through menopause (around age 50). Uterine fibroids can stay the same for years with few or no symptoms, or you can have a sudden, rapid growth of fibroids.
Fibroids do not grow before the start of menstrual periods (puberty). They sometimes grow larger during the first trimester of pregnancy, and they usually shrink for the rest of a pregnancy. After menopause, when hormone levels drop, fibroids usually shrink and don't come back.
Complications of uterine fibroids
Complications of uterine fibroids aren't common. Some of the problems that may happen are:
- Anemia from heavy bleeding.
- Problems with the urinary tract or bowels, if a fibroid presses on them.
- Infertility, especially if the fibroids grow inside the uterus and change the shape of the uterus.
- Ongoing low back pain or a feeling of pressure in the lower abdomen (pelvic pressure).
- Breakdown of uterine fibroid tissue. This can cause pain.
Fibroids may cause problems during pregnancy, such as:
- Preterm labor and delivery.
- Pain during the second and third trimesters.
- An abnormal fetal position, such as breech position, at birth.
- Placenta problems.
When to Call a Doctor
Call your doctor to make an appointment if you have:
- Heavy menstrual bleeding.
- Periods that have changed from relatively pain-free to painful over the past 3 to 6 months.
- Frequent painful urination, or you can't control the flow of urine.
- A change in the length of your menstrual cycle over 3 to 6 menstrual cycles.
- New persistent pain or heaviness in the lower belly or pelvis.
Exams and Tests
To find out if you have fibroids, your doctor will ask you about your symptoms and your menstrual periods. Your doctor will do a pelvic exam to check the size of your uterus.
You may get an ultrasound or another type of test that shows pictures of your uterus. These help your doctor see how large your fibroids are and where they are growing.
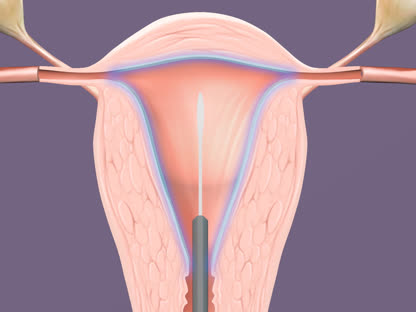
Your doctor may also do blood tests to look for anemia or other problems. You may have a hysteroscopy. This lets your doctor check the inside of your uterus. And sometimes an MRI is used before surgery to check the size and location of the fibroids.
Learn more
Treatment Overview
If your fibroids aren't bothering you, you don't need to do anything about them. Your doctor may check them during your regular visits to see if they have gotten bigger.
But if you have a fibroid problem, there are several treatments to consider. What treatment you choose may depend on how bad your symptoms are, if you want to get pregnant, and how close you are to menopause.
Medicines
Medicines are used to relieve symptoms like heavy menstrual bleeding or painful periods. These medicines include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs). They can improve menstrual cramping and reduce bleeding.
- Birth control hormones (pill, patch, or ring). They lighten menstrual bleeding and pain while preventing pregnancy.
- An intrauterine device (IUD) that releases small amounts of progestin into the uterus. It may reduce heavy menstrual bleeding.
- A progestin shot (Depo-Provera) every 3 months. It may lighten your bleeding.
- Tranexamic acid. This is a medicine that can reduce bleeding by helping blood to clot.
- Gonadotropin-releasing hormone analogue (GnRH-a) therapy. This shrinks the fibroids. It may be used to shrink fibroids before surgery. It can also help with symptoms.
- Iron supplements. They can help correct anemia caused by fibroid blood loss.
Procedures and surgery
If you have fibroid-related pain, heavy bleeding, or a large fibroid that is pressing on other organs, there are treatments you can try that shrink or remove your fibroids. After all treatments except hysterectomy, fibroids may grow back or new fibroids can grow. If you plan to get pregnant, talk with your doctor about which treatment is right for you.
- Shrinking or destroying fibroids without surgery.
- Uterine fibroid embolization stops the blood supply to the fibroid. The fibroid then shrinks.
- MRI-guided focused ultrasound uses high-intensity ultrasound waves to destroy the fibroids.
- Surgery to remove fibroids.
This surgery is called myomectomy. It preserves the uterus. This means you may be able to get pregnant in the future.
- Surgery to remove the entire uterus.
This surgery is called hysterectomy. It may be an option if you have no future pregnancy plans.
For infertility and pregnancy problems
Fibroids don't often affect fertility. But if a fibroid distorts the wall of the uterus, it can prevent a fertilized egg from implanting in the uterus. Surgery to remove the fibroid may improve your chances of getting pregnant.
When nearing menopause
If you are nearing menopause and can tolerate your symptoms, you can try to control them with home treatment and medicine. After menopause, your estrogen and progesterone levels will drop. This causes most fibroids to shrink and symptoms often improve.
Learn more
Watch
Self-Care
Try one or more of these tips to help relieve your menstrual pain.
- Ask your doctor if you can take nonsteroidal anti-inflammatory drugs (NSAIDs).
NSAIDs help relieve menstrual cramps and pain. Examples include ibuprofen and naproxen.
- Put heat on your lower belly.
Use a heating pad or hot water bottle, or take a warm bath. Heat improves blood flow and may ease pelvic pain.
- Elevate your legs.
Lie down and prop up your legs by putting a pillow under your knees. This may help relieve pain.
- Lie on your side, and bring your knees up to your chest.
This will help relieve back pressure.
- Get exercise.
Exercise improves blood flow and may reduce pain.
Learn more
Watch
Medicines
Medicine can be used to help relieve uterine fibroid problems. But when treatment is stopped, symptoms usually return.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) may help with menstrual cramping and heavy bleeding.
- Birth control hormones (pill, patch, or ring) reduce heavy menstrual periods and pain.
- An IUD that releases small amounts of a certain hormone (levonorgestrel) may reduce heavy menstrual bleeding.
- A progestin shot (Depo-Provera) may lighten your bleeding.
- Tranexamic acid is a medicine that can reduce bleeding by helping blood to clot.
- Iron supplements can help anemia.
- Gonadotropin-releasing hormone analogue (GnRH-a) therapy may be used to shrink fibroids before surgery. It can also help with symptoms. This treatment is used for a limited amount of time because it can weaken the bones.
Learn more
Surgery
Surgery can be used to remove uterine fibroids only (myomectomy). Or it can be used to remove the entire uterus (hysterectomy).
Surgery is an option when:
- You still have heavy uterine bleeding or anemia after several months of treatment.
- Fibroid pain or pressure affects your quality of life.
- The fibroids cause urinary or bowel problems.
- There is a chance that you have cancer.
- Fibroids may be making it hard to get pregnant.
Surgery choices
Options include:
- Myomectomy. This is surgery to remove the fibroids. If you hope to get pregnant later, myomectomy is your one surgical option.
- Hysterectomy. This is surgery to remove the uterus. It may be an option if you have no future plans to get pregnant.
Learn more
Watch
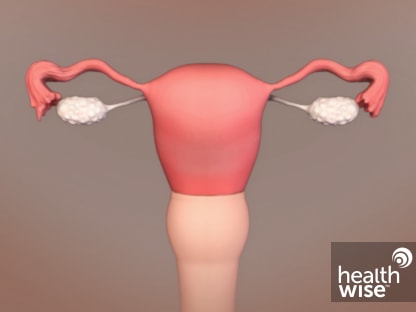
Uterine Fibroid Embolization (UFE)
Uterine fibroid embolization (UFE) shrinks or destroys uterine fibroids. It does this by blocking the artery that supplies blood to them.
This procedure is also called uterine artery embolization.
During UFE, a doctor places a thin, flexible tube called a catheter into the upper thigh. It is guided into the uterine artery that supplies blood to the fibroids. A liquid is then injected into the uterine artery through the catheter.
UFE is a nonsurgical option to hysterectomy or myomectomy. It relieves most fibroid symptoms. But in rare cases it can lead to problems, such as infection or early menopause.
UFE may be an option when:
- You don't want to get pregnant in the future. It's possible to get pregnant after UFE. But there may be risks.
- You still have heavy uterine bleeding or anemia after several months of treatment with birth control hormones and a nonsteroidal anti-inflammatory drug (NSAID).
- You have fibroid pain or pelvic pressure that affects your quality of life.
- You have urinary or bowel problems from a fibroid that is pressing on your bladder, ureter, or bowel.
- You don't want to have a hysterectomy or myomectomy.
- You have a disease or disorder that makes surgery with general anesthesia dangerous.
You can still get pregnant after UFE. If you need to prevent pregnancy after UFE, use birth control.
Learn more
Credits
Current as of: April 30, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: April 30, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.
To learn more about Ignite Healthwise, LLC, visit webmdignite.com.
© 2024-2025 Ignite Healthwise, LLC.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.