Pelvic Organ Prolapse
Make an Appointment
Our team is here to help you make an appointment with the specialists that you need.
Pelvic Organ Prolapse
Condition Basics
What is pelvic organ prolapse?
Pelvic organ prolapse means that a pelvic organ—such as your bladder—has moved from its normal position and is pressing against your vagina. This can happen when the muscles and tissues that hold your pelvic organs in place get weak or damaged.
Pelvic organ prolapse is common. It isn't usually a big health problem, but it can be uncomfortable or painful. It can be treated if it bothers you. And it may get better with time.
More than one pelvic organ can prolapse at the same time. Organs that can be involved include the:
- Bladder.
- Urethra.
- Uterus.
- Vagina.
- Small bowel.
- Rectum.
Female pelvic anatomy
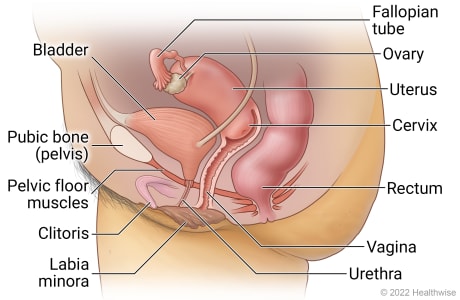
The pelvis is the ring of bones between the hips where several organs and structures are located. The female pelvic area includes the fallopian tubes, ovaries, uterus, cervix, bladder, urethra, pelvic floor muscles, clitoris, vagina, and rectum.
What causes it?
Pelvic organ prolapse occurs when the muscles and tissues that hold your pelvic organs in place get weak or damaged. It's often linked to pregnancy and vaginal childbirth. During pregnancy and delivery, pelvic muscles can get stretched and injured. Other causes of prolapse include aging, menopause, obesity, and frequent constipation.
What are the symptoms?
You may not have any symptoms. Or you may feel pressure from pelvic organs pressing against the vaginal wall. Your lower belly may feel very full, and you may feel as if something is falling out of your vagina. You may have urinary or bowel problems or pain during intercourse.
How is it diagnosed?
Your doctor will ask you questions about your past and current health. This includes asking about your symptoms and past pregnancies. Your doctor will also do a physical exam, including a pelvic exam. And you may have other tests. Pelvic organ prolapse that doesn't cause symptoms may be found during a routine exam.
How is pelvic organ prolapse treated?
You may not need or want treatment. But if symptoms bother you, you can try doing Kegel exercises and staying at a healthy weight. You can also try a pessary. Surgery may also be an option.
Cause
Pelvic organ prolapse occurs when the muscles and tissues that hold your pelvic organs in place get weak or damaged. It is often linked to pregnancy and childbirth. During pregnancy and vaginal delivery, pelvic muscles can get stretched and injured. If the muscles don't recover, they can't support your pelvic organs as well.
Anything that puts pressure on your belly can also increase your risk for pelvic organ prolapse. Things that can put pressure on your belly include obesity, frequent constipation, a long-lasting (chronic) cough, and frequent heavy lifting.
Pelvic organ prolapse can occur when you're young. But it's more likely to happen as you get older. And it's more common after menopause. It also tends to run in families.
Symptoms
You may not have any symptoms. Or pressure on your vagina may cause discomfort or problems with your pelvic organs. Symptoms may include:
- Feeling pressure or fullness in your lower belly.
- Feeling as if something is actually falling out of your vagina.
- Feeling a pull or a stretch in the groin area or a low backache.
- Pain during intercourse.
- Urinary problems. For example, you may release urine without meaning to (incontinence). Or you may have a frequent or urgent need to urinate.
- Problems with bowel movements. You may be constipated or need to support the back (posterior) of the vaginal wall to have a bowel movement.
Symptoms are worse when you stand, jump, or lift. They usually are relieved if you lie down.
When to Call a Doctor
Call your doctor to schedule an appointment if:
- You notice tissue pushing into your vagina or out of your vagina.
- You feel pulling or increased pelvic pressure that gets worse when you strain or lift but feels better when you lie down.
- Pain in your low back or pelvic area is interfering with your daily activities.
- Sexual intercourse has become difficult or painful.
- You have irregular spotting or bleeding from the vagina.
- You have urinary symptoms, such as involuntary release of urine (incontinence), urinating often, having an urgent need to urinate, or urinating often at night, that interfere with your daily activities.
- You have trouble having a bowel movement.
Watchful waiting
Watchful waiting is a wait-and-see approach. If you have been diagnosed with pelvic organ prolapse and you don't have symptoms, or if you have mild symptoms that aren't interfering with your daily activities, you may wish to try watchful waiting. In many cases, pelvic organ prolapse doesn't cause symptoms and doesn't need treatment.
If you have symptoms, such as a feeling of pressure in your vagina, schedule an appointment with your doctor.
Exams and Tests
A prolapse of a pelvic organ can be hard to diagnose. Pelvic organ prolapse that doesn't cause symptoms may be found during a routine exam. You may be aware that there's a problem, but you might not be sure of the exact location or cause. If your doctor thinks you may have an organ prolapse, your doctor will ask you questions about your past and current health. This includes questions about your symptoms and your history of pregnancies and other health problems. Your doctor will also do a physical exam, including a pelvic exam.
Tests may be done to find out more about the prolapse, particularly if it's causing problems with bladder or bowel function. These may include urodynamic tests and imaging tests, such as ultrasound or MRI.
Learn more
Watch
Treatment Overview
Decisions about treating pelvic organ prolapse are based on which organs have prolapsed and how bad your symptoms are. You may not need or want treatment.
If your symptoms are mild, you may be able to relieve them at home.
- Try Kegel exercises. These can make your pelvic muscles stronger.
- Reach and stay at a healthy weight.
- Avoid lifting heavy things. This can put stress on your pelvic muscles.
If these changes don't help, you can ask your doctor to fit you with a pessary. It's a removable device that you can put in your vagina to support areas of prolapse.
Surgery may be an option if symptoms don't get better with other treatments or if you prefer surgery over other treatments. But you may want to delay surgery if you plan to get pregnant in the future. The strain of childbirth could cause the prolapse to come back.
Self-Care
Home treatment can relieve the discomfort of pelvic organ prolapse. It can also help to keep prolapse from getting worse.
- Do Kegel exercises every day to strengthen the muscles and ligaments of the pelvis.
- Ask your doctor about a vaginal pessary. You can place this in your vagina to help support your pelvic organs. Your doctor can teach you how and when to remove, clean, and reinsert it.
- Prevent constipation. Straining caused by constipation increases pressure from the bowel on the vaginal wall and weakens and damages the connective tissue and muscles in the pelvis.
- Stay at a weight that’s healthy for you.
- Avoid activities that stress your pelvic muscles, such as heavy lifting.
- Try lying down with a pillow under your knees. This eases pressure on your vagina. You also can lie on your side and bring your knees up to your chest.
- Take care of your mental health, and get support if you need it. Pelvic organ prolapse can affect many aspects of your life, including your mental health. Talk to your doctor if you are feeling sad or anxious and it is not getting better. Support can also come from a counselor, support group, or trusted friend or family member.
Learn more
Watch
Surgery
If you have pain and discomfort from pelvic organ prolapse that isn't helped by nonsurgical treatment and lifestyle changes, you may want to think about surgery. Which type of surgery depends upon which organs are involved, how bad your symptoms are, and what other medical conditions you have. Also, your surgeon may have experience with and prefer to do a certain procedure. The goals of surgery are to relieve your symptoms and restore the normal functioning of your pelvic organs. Types of surgeries used to correct pelvic organ prolapse may include:
- Reconstructive surgery. This surgery helps repair and support the vaginal wall and bring pelvic organs back to their original position.
- Vaginal obliteration. This closes the vagina to help support the prolapsed organs.
- Hysterectomy. Removal of the uterus.
These surgeries can help treat your symptoms. But some people may have symptoms of urinary incontinence after surgery. Your doctor may do an exam to check if urinary incontinence could be a problem for you after surgery. If the exam shows that it could be a problem, surgery to correct stress urinary incontinence can be done at the same time as surgery to repair prolapse.
Learn more
Watch
Credits
Current as of: October 19, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.
To learn more about Ignite Healthwise, LLC, visit webmdignite.com.
© 2024-2025 Ignite Healthwise, LLC.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.

