Peripheral Arterial Angioplasty
Make an Appointment
Our team is here to help you make an appointment with the specialists that you need.
Peripheral Arterial Angioplasty
Procedure Overview
Peripheral artery angioplasty (say "puh-RIFF-er-rull AR-ter-ree ANN-jee-oh-plass-tee") is a procedure to treat peripheral arterial disease of the legs. The procedure widens narrowed arteries in the pelvis or legs. It can help blood flow better. This may decrease leg pain or help wounds heal better.
Your arteries can get narrowed by a substance called plaque. Plaque is a buildup of fats in your arteries.
You may be asleep for the procedure. Or you may be awake. You will get medicine to prevent pain and help you relax. First, your doctor will do a test to find narrowed arteries. Your doctor will put a tiny tube into an artery in your groin or wrist. This tube is called a catheter. The doctor moves the catheter through the artery and puts a dye into it. The dye makes your arteries show up on X-ray pictures. This lets the doctor see any narrowed parts of the arteries.
If your doctor finds a narrowed artery, they may do an angioplasty. To do this, the doctor uses a catheter with a balloon at the tip. It goes into the artery in your groin or leg. The doctor moves the balloon to the narrowed area and inflates it. The balloon presses the plaque against the walls of the artery. This makes more room for blood to flow. The doctor may also put a stent in your artery. A stent is a small tube that helps keep the artery open.
You may go home the same day. Or you may spend the night in the hospital. For 1 or 2 days after the procedure, you will need to take it easy at home.
How It Is Done
Iliac artery is narrowed by plaque
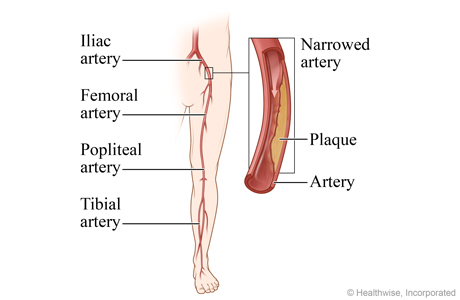
Angioplasty is used to open narrowed arteries and increase oxygen-rich blood flow to muscle and tissue. These images show angioplasty for the iliac artery. Angioplasty can also be done for the femoral, popliteal, and tibial arteries.
Catheter is inserted
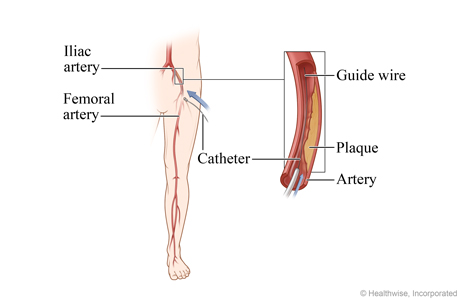
You may be asleep for the procedure. Or you may be awake. You will get medicine to prevent pain and help you relax. Then the doctor inserts a thin, flexible tube called a catheter into a blood vessel. In this image, the catheter is inserted into the femoral artery in the thigh and carefully guided to the narrowed part of the iliac artery. A wire inside the catheter is used to guide tools, including a small balloon, into the artery.
Balloon is inflated, stent is expanded
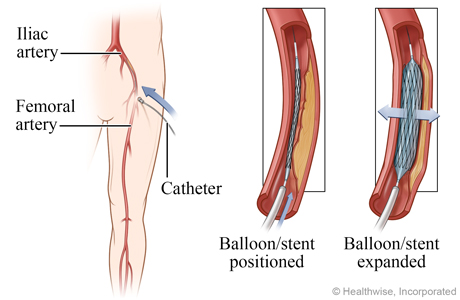
The doctor guides the catheter to the narrowed part of the artery and inflates a small balloon at the end of a tube. The balloon may remain inflated for a short time. If the doctor is going to place a stent in the artery, the balloon is inflated inside of the stent. The pressure from the inflated balloon causes the stent to expand and press the plaque against the wall of the artery, creating more room for blood to flow.
Balloon is removed, stent is in place
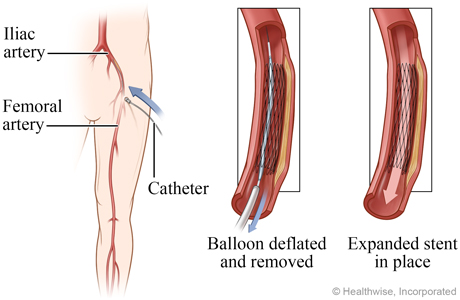
Next, the doctor deflates the balloon and removes it, leaving the expanded stent in place to keep the walls of the artery open.
Before and after angioplasty
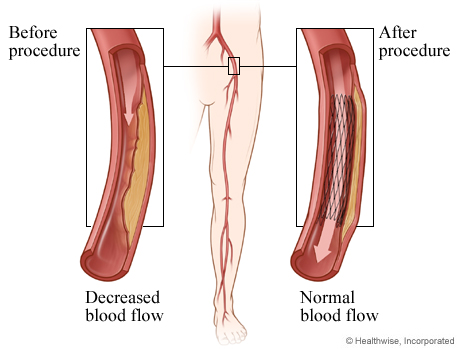
Angioplasty can widen a narrowed part of an artery. This increases the flow of oxygen-rich and nutrient-rich blood to the leg.
What to Expect
After the procedure, pressure may be applied to the area where the catheter was put into your blood vessel. This will help prevent bleeding. A small device may also be used to close the blood vessel. The area may be covered with a bandage or a compression device.
If the catheter was put in your groin, you will keep your leg still for up to a few hours. If it was put in your wrist, you may need to keep your arm still for 2 hours.
You may go home the same day. Or you may stay overnight in the hospital. Don't do anything strenuous until your doctor says it's okay. This may be for several days. You may have a bruise or small lump where the catheter was put in your blood vessel. This is normal and will go away.
You will likely have regular checkups with your doctor to check your arteries.
Why It Is Done
This procedure is used to improve blood flow in narrowed arteries that supply blood to the legs and feet. It may be used on short sections of narrowed arteries in people who have peripheral arterial disease (PAD).
How Well It Works
Peripheral artery angioplasty can improve blood flow and relieve intermittent claudication.footnote 1, footnote 2, footnote 3 Angioplasty may help you walk farther without leg pain than you did before the procedure.footnote 4
How well angioplasty works depends on the size of the blood vessel, the length of blood vessel affected, and whether the blood vessel is completely blocked.
In general, angioplasty works best in:
- Larger arteries.
- Arteries with short narrowed areas.
- Narrowed, not blocked, arteries.
Risks
Complications related to the catheter include:
- Pain, swelling, and tenderness at the catheter insertion site.
- Bleeding at the catheter site.
- A bruise where the catheter was inserted. This usually goes away in a few days.
Serious complications are rare. These complications may include:
- Closure of the artery.
- Blood clots.
- A small tear in the inner lining of the artery.
- An allergic reaction to the contrast material used to view the arteries.
- Kidney damage. In rare cases, the contrast material can damage the kidneys, possibly causing kidney failure.
Over time, blood vessels with stents may become narrow again.
Radiation risk
There is always a slight risk of damage to cells or tissues from being exposed to any radiation, including the low levels of X-ray used for this test. But the risk of damage from the X-rays is usually very low compared with the potential benefits of the test.
References
Citations
- Gerhard-Herman MD, et al. (2016). 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease. Circulation, published online November 13, 2016. DOI: 10.1161/CIR.0000000000000471. Accessed November 25, 2016.
- Conte M, et al. (2015). Society for Vascular Surgery practice guidelines for atherosclerotic occlusive disease of the lower extremities: Management of asymptomatic disease and claudication. Journal of Vascular Surgery, 61(3S): 2S–41S. DOI: 10.1016/j.jvs.2014.12.009. Accessed November 25, 2016.
- Conte MS, et al. (2019). Global vascular guidelines on the management of chronic limb-threatening ischemia. Journal of Vascular Surgery, 69(6S): 3S–125S.e40. DOI: 10.1016/j.jvs.2019.02.016. Accessed June 1, 2023.
- Fakhry F, et al. (2018). Endovascular revascularization versus conservative management for intermittent claudication. Cochrane Database of Scientific Reviews (3). DOI: 10.1002/14651858.CD010512.pub2. Accessed April 13, 2018.
Credits
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.
To learn more about Ignite Healthwise, LLC, visit webmdignite.com.
© 2024-2025 Ignite Healthwise, LLC.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.



